Joseph Cirrone, MD, Radiation Oncologist
History & Presentation
The patient is a 68-year-old white male with a past medical history significant for hypertension and hypercholesterolemia.
Patient had a routine physical examination with screening PSA performed in October of 2013. The PSA was noted to be 5.5 ng/ml. The patient was sent for urologic evaluation. A prostate biopsy was performed on December 16, 2013. One of twelve (1/12) cores was positive for invasive adenocarcinoma. The Gleason score was 7 (4+3). There was associated perineural space invasion. The patient had staging evaluation with CT scan of the abdomen and pelvis without evidence of metastatic disease.
The patient was given treatment options by his urologist, and surgery was to be considered. The patient sought a second urologic evaluation at Memorial Sloan-Kettering Cancer Center. The pathology slides were reviewed and again found to be adenocarcinoma of the prostate with a Gleanson of 7, but this time the major and minor components were switched where 3 was major and 4 was the minor Gleason score. The patient was informed by Memorial Sloan-Kettering Cancer physician that surgery was an option but also radiation therapy could be considered in his case. The patient was hesitant to have definitive surgery, and he has been referred to consider definitive radiation therapy for his newly diagnosed prostate cancer.
Treatment Options
Patient was given multiple definitive treatment options for early stage, intermediate risk prostate cancer. Options included: observation; hormonal therapy; external beam radiation therapy, usually with combined hormone therapy or alone or with IGRT technique over 9 weeks; or CyberKnife radiotherapy given in five treatments every other day. Patient was told the exact procedure for each option and specific side effects.
Treatment
The patient opted for definitive therapy using the Precision CyberKnife (PCK) Radiotherapy treatment. In November 2014, patient has his initial consult at PCK and subsequently received the five treatments as outlined to a total dose of 3500 cGy, each daily treatment lasting approximately 40 minutes. Patient completed the therapy without complaints.
Post Treatment
For the next two weeks post treatment patient had mild urinary frequency/pressure and mild fatigue. After a month, patient’s urination returned to normal and returned to his baseline activity level.
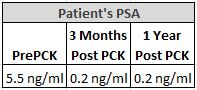
Three months later he was seen in follow-up, repeat PSA was 0.2 ng/ml compared to the patient’s pre-treatment PSA 5.5 ng/ml.
One year later the patient remains clinically well without complaints, the PSA remains low at 0.2 ng/ml.

