Here’s what you need to know about the new lung cancer screening guidelines
Do you currently smoke or are you a former smoker? If so, you may benefit from an annual lung cancer screening. Cigarette smoking is the leading cause of lung cancer and according to the CDC, lung cancer is the third most common type of cancer and the leading cause of cancer-related death in the United States. It kills more people each year than breast, prostate, and colon cancers combined.
What are the symptoms of lung cancer?
With lung cancer, by the time you have symptoms – usually a persistent cough along with shortness of breath or wheezing – the disease is already more advanced and harder to treat. That’s why it’s so important to detect lung cancer as early as possible with screenings.
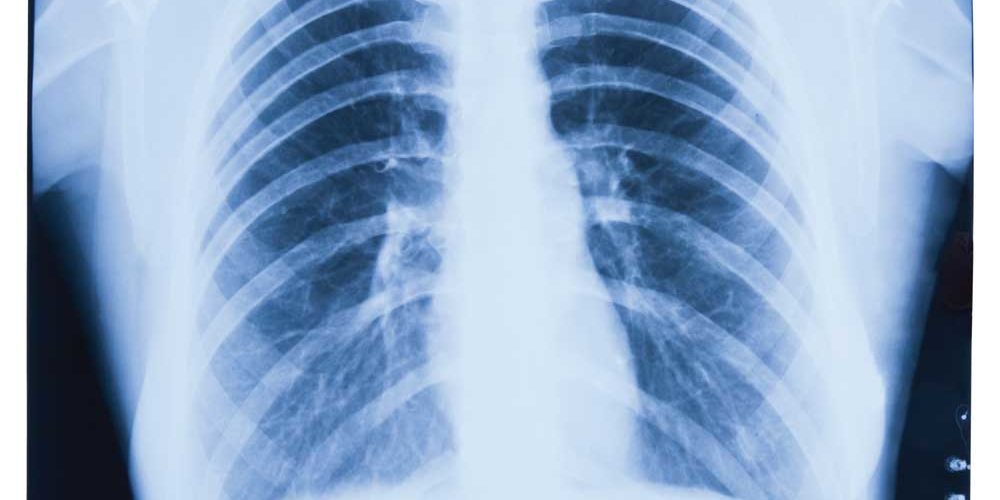
What is a lung cancer screening?
The test is a low-dose CT scan of your chest and there’s no prep needed for this screening. If your test results are negative, then it will likely be recommended that you come back annually for screening. If something is seen on your scan, it’s important not to panic. This does not mean that you have lung cancer. For example, if you have pneumonia, the finding on the CT scan may look very similar to lung cancer. It is also common for the scan to show lung nodules, which often are not cancerous. Usually, follow-up tests will be conducted to differentiate between benign and malignant conditions. “We now have a proven tool to screen for lung cancer… like mammograms for breast cancer and colonoscopy for colon cancer,” said Jay M. Barbakoff, MD, Northwell Health Pulmonary Physicians at Port Jefferson. “Early detection leads to much higher survival rates than when patients present with symptoms. ALL high-risk patients should get yearly low dose radiation CT chest screening.”
What are the changes to the screening guidelines?
In March 2021, the United States Preventative Services Task Force (USPSTF) updated their lung cancer screening guidelines. In the new guidelines, both the quantity of tobacco consumed and the age eligibility for screening were lowered. Lung cancer screening is now recommended for individuals aged 50 to 80 years who have a 20 pack-year smoking history. Most insurance companies will cover lung cancer screening for people who fit these guidelines and are considered at high risk.
What is a pack-year?
A pack year is an estimate of how much you’ve smoked in your lifetime by multiplying packs of cigarettes smoked per day by the number of years you smoked. One pack-year means you smoked about one pack (20 cigarettes) every day for a year. If you smoked a pack a day for 20 years, that correlates to a 20 pack-year history.
Why change the screening guidelines?
By expanding the screening criteria, 6.5 million additional Americans will qualify for screening. Evidence from the USPSTF has shown that low-dose CT screening has effectively reduced lung cancer deaths by 20 to 33 percent which means that the increase in the number of people screened under these new guidelines has the potential to save an additional 10,000 to 20,000 lives each year.
Lung cancer screening not only detects early treatable lung cancers but also can detect abnormalities in other parts of the body such as the heart, aorta, thyroid, liver, and kidneys. By screening people who are younger and have smoked fewer cigarettes, more lives can be saved and people can live longer healthier lives.
How can I reduce my risk of lung cancer?
The best way you can reduce your risk of lung cancer is to quit smoking today. Even if you get an annual lung cancer screening, you should still quit smoking. There are smoking cessation programs that can help you quit by teaching you about the behavioral aspects of smoking and addressing your triggers. There are also seven FDA-approved smoking cessation medications that can assist you with quitting. Talk to your doctor today about how you can kick the habit.
Take our lung cancer risk assessment and see if you should get screened.